10 Different Types of Assisted Reproductive Technology (ART)
In the past, infertility was considered a permanent roadblock to having biological children. But today, assisted reproductive technology (ART) is revolutionizing the way we approach conception. As per the Centers for Disease Control and Prevention (CDC), over 2% of all births in the U.S. are now the result of ART, a number that continues to grow each year.
If you’re navigating fertility challenges, you’re not alone—and you have more options than ever before. In this comprehensive guide, we’ll explore the different types of ART, how each works, and when they might be right for you.
What Is Assisted Reproductive Technology (ART)?

ART refers to medical procedures that involve handling eggs, sperm, or embryos to help people conceive. It’s often recommended when natural conception has failed despite 6–12 months of unprotected intercourse, or when there’s a known fertility barrier (e.g., blocked fallopian tubes, male factor infertility, or age-related decline).
Different Types of Assisted Reproductive Technology (ART)
Unlike general fertility treatments (like hormone therapy), ART specifically involves egg retrieval, fertilization in the lab, and embryo transfer or implantation.
In Vitro Fertilization (IVF)
What is it?
IVF is the most well-known ART technique. It involves retrieving eggs from the ovaries, fertilizing them with sperm in a lab, and transferring the embryo into the uterus.
Steps
- Ovarian stimulation with fertility drugs
- Egg retrieval via ultrasound-guided aspiration
- Fertilization of eggs in the lab
- Embryo culture for 3–5 days
- Embryo transfer into the uterus
- Pregnancy test after 10–14 days
Ideal for
- Blocked or damaged fallopian tubes
- Unexplained infertility
- Endometriosis
- Male factor infertility
Success rate: Varies with age: up to 50% per cycle in women under 35.
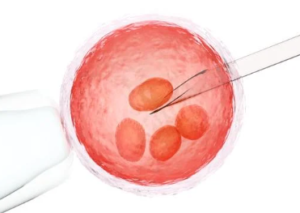
Intracytoplasmic Sperm Injection (ICSI)
What is it?
ICSI is a specialized form of IVF where a single sperm is directly injected into an egg.
When is it used?
- Severe male infertility (low count, poor motility)
- Prior IVF failures
- Obstructive azoospermia (no sperm in ejaculate)
Why it works: By bypassing the natural barrier to sperm entry, ICSI increases the odds of fertilization in difficult cases.
Intrauterine Insemination (IUI)
What is it?
Also called artificial insemination, IUI involves placing sperm directly into the uterus around ovulation time.
Steps
- Ovulation monitoring (with or without fertility meds)
- Sperm collection and preparation
- Sperm insertion via a thin catheter
Ideal for
- Mild male infertility
- Cervical mucus issues
- LGBTQ+ families and single women using donor sperm
Success rate: Around 10–20% per cycle, depending on age and diagnosis.
Pros: IUI is less invasive and more affordable than IVF, often used as a first-line ART option.
Gamete Intrafallopian Transfer (GIFT)
What is it?
GIFT involves retrieving eggs and sperm and placing them directly into the fallopian tube, where fertilization occurs naturally.
Key Point: Unlike IVF, fertilization happens inside the body, not in a lab.
Requirements: Healthy, unblocked fallopian tubes
Less commonly used today, GIFT has largely been replaced by IVF due to its higher control and success rates.
Zygote Intrafallopian Transfer (ZIFT)
What is it?
ZIFT is a hybrid of IVF and GIFT. Eggs are fertilized in the lab (like IVF), but instead of placing embryos in the uterus, they’re transferred into the fallopian tube at the zygote stage (24 hours post-fertilization).
Why choose ZIFT?
- Preference for natural implantation
- Ethical or religious beliefs against lab embryo culture
Like GIFT, ZIFT is rarely used today due to the more invasive procedure and limited advantage over IVF.
Frozen Embryo Transfer (FET)

What is it?
FET involves thawing and transferring embryos that were previously frozen, often from an earlier IVF cycle.
Benefits
- Saves extra embryos from previous cycles
- Allows for PGT (genetic testing)
- Reduces physical and emotional stress
- Useful in “freeze-all” IVF strategies to avoid OHSS
Success rate: FET success rates match or exceed fresh transfers in many cases.
Donor Eggs and Donor Sperm
When is it needed?
- Premature ovarian failure
- Age-related decline in egg quality
- Genetic conditions
- Severe male infertility (for sperm donation)
Process
- Sourcing donor eggs/sperm from a certified bank
- Synchronizing donor cycle (for eggs)
- IVF with donor gametes
Considerations
- Legal agreements
- Emotional impact
- Anonymity and future disclosure
Donor gametes offer a high success rate, especially with young, healthy donors.
Gestational Surrogacy (Carrier)
What is it?
A gestational carrier (surrogate) carries a pregnancy for another person or couple. The embryo is created via IVF using the intended parent’s or donor’s egg/sperm and implanted into the surrogate’s uterus.
Used for
- Uterine abnormalities
- Repeated implantation failure
- Health risks to the intended mother
- LGBTQ+ male couples or single men
Legal considerations: Surrogacy laws vary by country and state. Contracts are essential to protect all parties involved.
Preimplantation Genetic Testing (PGT)

What is it?
PGT screens embryos for genetic or chromosomal abnormalities before implantation.
Types
- PGT-A: Tests for aneuploidy (extra or missing chromosomes)
- PGT-M: Screens for monogenic (single gene) disorders
- PGT-SR: Identifies structural rearrangements
Benefits
- Reduces miscarriage risk
- Increases success in older women
- Helps prevent inherited conditions
PGT is often used with IVF, especially in high-risk couples or repeated IVF failures.
Assisted Hatching
What is it?
A lab technique that thins or opens the embryo’s outer shell (zona pellucida) to help it hatch and implant in the uterus.
Recommended for
- Women over 37
- Frozen embryos
- Previous IVF failures
Though somewhat controversial, some studies suggest it improves implantation in certain patients.
Emerging and Experimental ART Techniques
Several next-generation reproductive technologies are in development:
- In Vitro Maturation (IVM): Maturing eggs outside the body, useful for PCOS patients
- Mitochondrial Replacement Therapy (MRT): Prevents mitochondrial diseases by combining DNA from 3 people
- Uterine Transplants: For women born without a uterus or with uterine disease
- Artificial Gametes: Using stem cells to create sperm or eggs (in experimental stages)
These options could reshape fertility medicine in the next decade.
Risks and Challenges of ART
Like any medical procedure, ART has potential risks:
- Multiple pregnancies (twins or triplets)
- Ovarian hyperstimulation syndrome (OHSS)
- Emotional and financial stress
- Ethical and legal dilemmas
- Higher risk of preterm birth and low birth weight
Choosing the right ART requires individualized medical advice from a fertility specialist.
Conclusion: Finding the Right Path to Parenthood
Choosing among the different types of assisted reproductive technology can feel overwhelming—but you’re not alone. With the right medical team, support system, and knowledge, ART can help make your dream of parenthood a reality.
Whether it’s IVF, ICSI, or donor options, every journey is unique. Consult with a fertility specialist to evaluate your options, address your needs, and take confident steps toward conception.
FAQ – Different Types of Assisted Reproductive Technology

Are there different types of IVF?
Yes, there are several variations of IVF, each tailored to suit specific medical needs and personal preferences:
- Conventional IVF: The standard method where eggs and sperm are combined in a lab and observed for fertilization.
- Natural Cycle IVF: No fertility drugs are used. One naturally ovulated egg is retrieved and fertilized.
- Mini IVF (Mild Stimulation IVF): Uses lower doses of fertility drugs to produce fewer eggs, reducing side effects and cost.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected into each egg—ideal for male infertility.
- Frozen Embryo Transfer (FET): Embryos from a previous cycle are thawed and transferred.
- Donor IVF: Involves donor eggs or sperm for couples unable to produce their own viable gametes.
Each type has specific indications and success rates, depending on the individual or couple’s fertility condition.
What are the four types of artificial insemination?
Artificial insemination involves placing sperm into a woman’s reproductive tract to increase the chances of pregnancy. The four main types are:
- Intrauterine Insemination (IUI): The most common method; sperm is placed directly into the uterus.
- Intracervical Insemination (ICI): Sperm is placed at the opening of the cervix; commonly used for at-home insemination.
- Intratubal Insemination (ITI): Less commonly used; sperm is introduced directly into the fallopian tubes.
- Intravaginal Insemination (IVI): Sperm is deposited into the vaginal canal, mimicking natural intercourse.
IUI is generally the most effective and commonly used in clinical settings.
What are the 4 stages of IVF?
IVF typically involves four main stages:
- Ovarian Stimulation: Fertility drugs are used to stimulate the ovaries to produce multiple eggs.
- Egg Retrieval: Eggs are collected from the ovaries using a minimally invasive procedure.
- Fertilization and Embryo Culture: Eggs are fertilized with sperm in a lab, and the resulting embryos are cultured.
- Embryo Transfer: The best-quality embryo(s) are transferred into the uterus for potential implantation and pregnancy.
A pregnancy test is conducted about two weeks after the transfer to confirm success.
What are the disadvantages of IVF babies?
While most IVF-conceived babies are healthy, there are some considerations and potential disadvantages:
- Slightly Increased Risk of Birth Defects: Studies suggest a minor increase, though the absolute risk remains low.
- Higher Likelihood of Preterm Birth and Low Birth Weight: Especially in cases of multiple embryo transfers.
- Cost and Accessibility: IVF can be expensive and is not always covered by insurance.
- Emotional Stress: The process can be physically and emotionally demanding for individuals and couples.
However, most risks are manageable and should be discussed with a healthcare provider.
Who is the father of artificial insemination?
The title of “father of artificial insemination” is often attributed to Spallanzani Lazzaro, an Italian biologist from the 18th century. In 1784, he successfully performed the first documented case of artificial insemination in a dog, demonstrating that fertilization could occur without natural intercourse. His work laid the groundwork for the development of modern reproductive technologies.






