Advanced Testing for a Clearer Path to Conception
Unlock the Key to Parenthood with Comprehensive Fertility Diagnostics

Schedule Your Fertility Assessment Today
Infertility is a medical condition characterized by the inability to conceive despite actively trying for 12 months of regular, unprotected intercourse. For women over the age of 35, this timeframe shortens to 6 months due to age-related fertility decline.
It’s a challenge that affects millions globally, with men and women contributing equally to the statistics. While the causes can vary, infertility often stems from underlying issues like hormonal imbalances, reproductive abnormalities, or environmental factors.
The Impact of Infertility
Infertility is more than just a physical hurdle—it touches every aspect of life. The emotional weight of being unable to conceive can lead to stress, anxiety, and even depression. Relationships may feel strained as couples navigate the uncertainties and frustrations of fertility challenges. Many individuals experience feelings of isolation, believing they are alone in their journey, despite the widespread prevalence of infertility.
However, early intervention can make a significant difference. By identifying the root causes and exploring personalized solutions, individuals and couples can regain hope. At Eva Fertility Clinic, we are committed to supporting you every step of the way—providing compassionate care, innovative treatments, and a path toward realizing your dream of parenthood. Infertility is not the end of your journey; it’s a step toward a solution.
The Role of Fertility Tests
- Fertility tests play a crucial role in unraveling the complexities of infertility, serving as the foundation for effective diagnosis and treatment.
- These tests provide vital information about the health of reproductive organs, hormonal balance, egg and sperm quality, and the overall ability to conceive.
- From ultrasounds and hormone level evaluations to advanced tests like DNA Fragmentation Index (DFI) and Endometrial Receptivity Assay (ERA), each assessment brings specialists closer to understanding your unique fertility profile.
- With this knowledge, fertility experts can craft personalized treatment plans tailored to your specific needs, increasing the likelihood of a successful outcome.
The Importance of Early Testing
- Early fertility testing is a game-changer, significantly improving the chances of conception and a healthy pregnancy.
- It helps detect underlying issues like hormonal imbalances, tubal blockages, or sperm abnormalities early, when they are more manageable.
- Timely intervention prevents minor problems from escalating into more complex challenges that could delay or hinder conception.
- Additionally, early testing offers emotional relief by providing clarity and actionable next steps, reducing the uncertainty and stress often associated with infertility.
- Timely testing is not just about identifying problems—it’s about reclaiming time, options, and the joy of moving closer to your dream of parenthood.
Types of Infertility
Infertility affects individuals and couples differently, and understanding its type is the first step toward effective treatment. Broadly, infertility is categorized into three types: Primary, Secondary, and Unexplained Infertility.
Primary infertility refers to the inability to conceive after one year of trying (or six months for women over 35) without any prior pregnancies. Common causes include:
- Ovulatory Disorders: Conditions like PCOS and hormonal imbalances disrupt ovulation, preventing the release of eggs.
- Uterine Abnormalities: Issues such as fibroids or endometriosis can interfere with implantation or pregnancy.
- Tubal Blockages: Damage or blockages in the fallopian tubes prevent eggs from meeting sperm, hindering fertilization.
For men, factors like low sperm count, poor motility, or structural abnormalities often contribute to primary infertility. Advanced diagnostics help identify these root causes to create a personalized treatment plan.
Secondary infertility occurs when an individual or couple struggles to conceive again after previously having a child. Though a prior successful pregnancy is reassuring, factors like age, lifestyle changes, or medical conditions may arise over time.
- For women, aging, uterine changes, or scarring from previous pregnancies or surgeries can impact fertility.
- For men, hormonal changes, declining sperm quality, or obstructions in the reproductive tract may develop.
Secondary infertility is just as emotionally challenging as primary infertility, and early intervention is critical to restoring the path to parenthood.
Unexplained infertility is diagnosed when standard tests fail to identify a clear cause. Despite the absence of obvious issues, couples still face difficulty conceiving.
Advanced diagnostic tools, such as the DNA Fragmentation Index (DFI) for sperm quality and the Endometrial Receptivity Assay (ERA) for uterine health, often uncover subtle factors that standard tests might miss.
With evolving technology and tailored treatments, unexplained infertility no longer means unanswered questions—it’s a starting point for deeper exploration and innovative solutions.
Types of Fertility Tests in EVA

Ultrasound
Learn more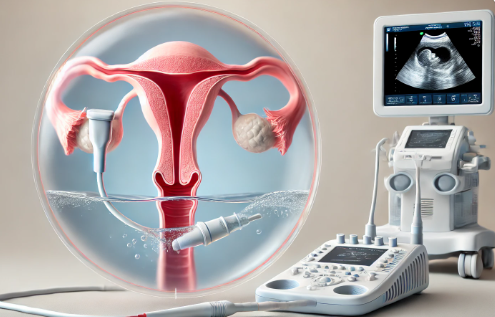
Saline Infusion Sonography (SSG)
Learn more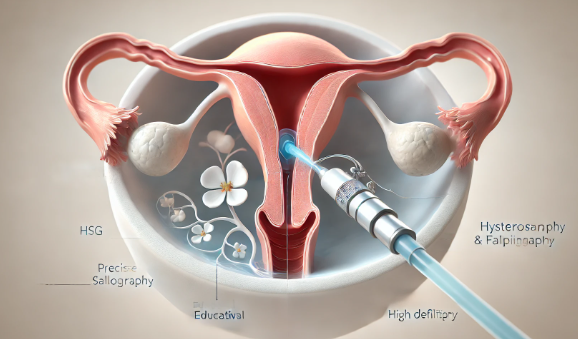
HysterosalPhingography (HSG)
Learn more
Sperm Function Tests
Learn more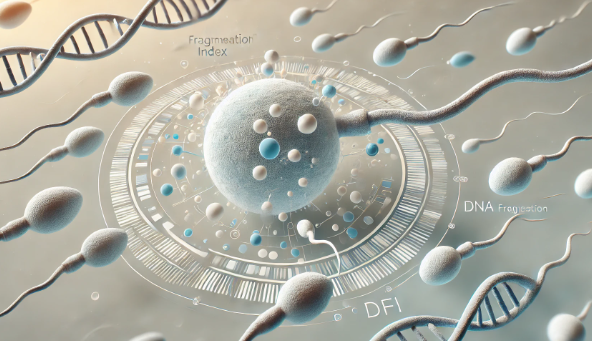
DNA Fragmentation Index (DFI)
Learn more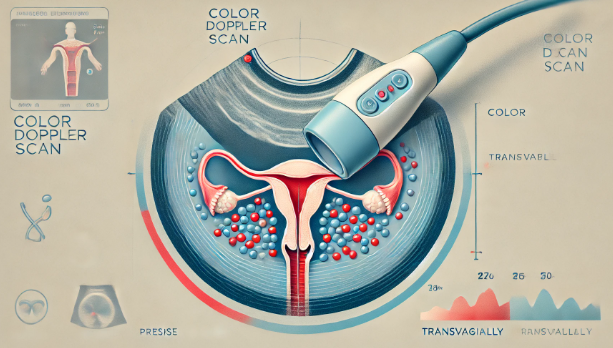
Color Doppler Scans
Learn more
Genetic Evaluations
Learn more
Previous IVF Failure Evaluation
Learn more
Endometrial Receptivity Assay (ERA)
Learn moreMaintaining Fertility Health
Why Fertility Health Matters?
Supports Reproductive Longevity: Maintaining optimal fertility health ensures that your reproductive system remains functional for a longer period, giving you more flexibility and options when planning a family.
Reduces Pregnancy Complications: A healthy reproductive system lowers the risk of pregnancy challenges, such as miscarriage, preterm labor, or conditions like gestational diabetes.
Enhances Overall Well-Being: Fertility health reflects your general health. Balanced hormones, proper nutrition, and reduced stress not only aid conception but also improve your mental and physical wellness.
Good fertility health is about more than reproduction—it’s about living a healthier, happier life overall.
Tips to Maintain Fertility Health
Maintain a Healthy Weight: Both underweight and overweight individuals can face fertility challenges. Aim for balanced nutrition with plenty of fruits, vegetables, whole grains, and lean protein.
Avoid Harmful Substances: Smoking, excessive alcohol consumption, and exposure to environmental toxins can harm sperm and egg quality. Eliminating these factors can dramatically improve reproductive outcomes.
Manage Stress: Chronic stress disrupts hormone production, impacting ovulation and sperm production. Practice mindfulness, meditation, or relaxation techniques to reduce stress and boost fertility.
Seek Early Testing: If conception is taking longer than expected, don’t wait. Early fertility testing can identify and address potential issues before they become major obstacles.
Did You Know?
Infertility is more common than many realize, affecting millions of individuals and couples worldwide. Here are some eye-opening facts to help you understand the prevalence and importance of addressing fertility challenges:
1. 1 in 6 Couples Experiences Infertility Globally
Research shows that infertility affects approximately 17% of couples worldwide, making it a significant global health concern. Despite its prevalence, many individuals face stigma or delay seeking help, often missing the opportunity for early intervention. By raising awareness and providing access to advanced care, we can ensure more couples receive the support they need.
2. Up to 30% of Infertility Cases Involve Both Male and Female Factors
Infertility is not solely a male or female issue. Studies reveal that 30% of cases stem from combined factors in both partners. This highlights the importance of evaluating both individuals in a couple when diagnosing and treating infertility. With comprehensive testing and collaborative care, fertility specialists can address these shared challenges effectively.
3. With Advanced Diagnostics, Over 85% of Couples Discover Actionable Causes
Modern fertility diagnostics have revolutionized the way we understand and treat infertility. Advanced tools such as DNA Fragmentation Index (DFI), Endometrial Receptivity Assay (ERA), and genetic evaluations uncover subtle yet critical factors impacting fertility. Remarkably, over 85% of couples undergoing these tests find actionable insights, enabling personalized treatments that dramatically increase their chances of conceiving.
Why These Statistics Matter?
Understanding these statistics underscores the importance of seeking timely, comprehensive fertility care. At Eva IVF & Women’s Centre, we’re dedicated to breaking down barriers and providing advanced diagnostics that turn these numbers into success stories. Infertility is not the end—it’s the beginning of a journey we’re here to support.
FAQ – Fertility Diagnostics
There isn’t a one-size-fits-all test for female fertility, as it often involves a combination of diagnostics. Commonly recommended tests include:
- Hormone Tests: Evaluate levels of hormones like FSH, LH, and AMH to assess ovarian reserve and ovulation.
- Ultrasound: Monitors ovarian follicles and checks for uterine abnormalities.
- Hysterosalpingography (HSG): Examines the health of fallopian tubes and the uterine cavity.
- Endometrial Receptivity Assay (ERA): Determines the best time for embryo implantation.
Egg quality isn’t measured directly, but several tests can provide valuable insights:
- AMH (Anti-Müllerian Hormone) Test: Indicates the quantity of eggs in the ovaries, indirectly reflecting quality.
- FSH (Follicle-Stimulating Hormone) Test: Higher levels may signal diminished egg quality.
- Ultrasound for Antral Follicle Count: Counts the number of follicles in the ovaries, a marker of ovarian reserve.
- IVF Embryo Assessment: During IVF, egg quality is observed through fertilization and embryo development.
While egg quality can only be confirmed through advanced fertility tests or IVF, there are some signs that may indicate potential issues:
- Irregular Menstrual Cycles: Suggesting hormonal imbalances that could impact egg development.
- Difficulty Conceiving: Despite regular attempts and no other identifiable factors.
- Recurrent Miscarriages: Poor egg quality can result in chromosomal abnormalities leading to pregnancy loss.
- Age-Related Fertility Decline: Women over 35 may naturally experience a reduction in egg quality.
Yes, AMH levels can decline within six months, especially as a woman ages or due to medical conditions like PCOS, endometriosis, or autoimmune diseases. However, slight fluctuations in AMH levels are normal and don’t always indicate a dramatic change in fertility. Lifestyle factors such as stress, poor diet, or smoking may also influence levels. Regular monitoring by a fertility specialist can help track these changes and guide appropriate interventions.
Yes, folic acid plays a crucial role in improving egg quality. It’s a key vitamin for DNA synthesis and repair, which is essential for healthy egg development and maturation. Taking a daily folic acid supplement not only enhances fertility but also reduces the risk of birth defects in early pregnancy. Combine folic acid with a balanced diet rich in leafy greens, citrus fruits, and fortified grains for the best results. A fertility specialist can recommend the right dosage tailored to your needs.
